Zahnfilm: neuropathischer Schmerz und Zahnschmerz im Fokus
Wenn Schmerzen im Mundraum auftreten, ist es meistens sehr unangenehm, da wir schließlich sehr stark auf diesen Bereich angewiesen sind, ob nun beim Essen, Trinken oder auch Sprechen. Die Schmerzen können unterschiedliche Ursachen haben, beispielsweise die Zähne, die Wurzeln, das Zahnfleisch oder auch den Kiefer. Vor allem Kieferschmerzen sind noch einmal eine besondere Form, der sich Experten aus der Zahnzunft widmen. Unter anderem auch auf der Webseite „Zahnfilm.de„, die von Joachim Wagner betrieben wird und sich in erster Linie den chronischen Schmerzen im Kiefer widmet.
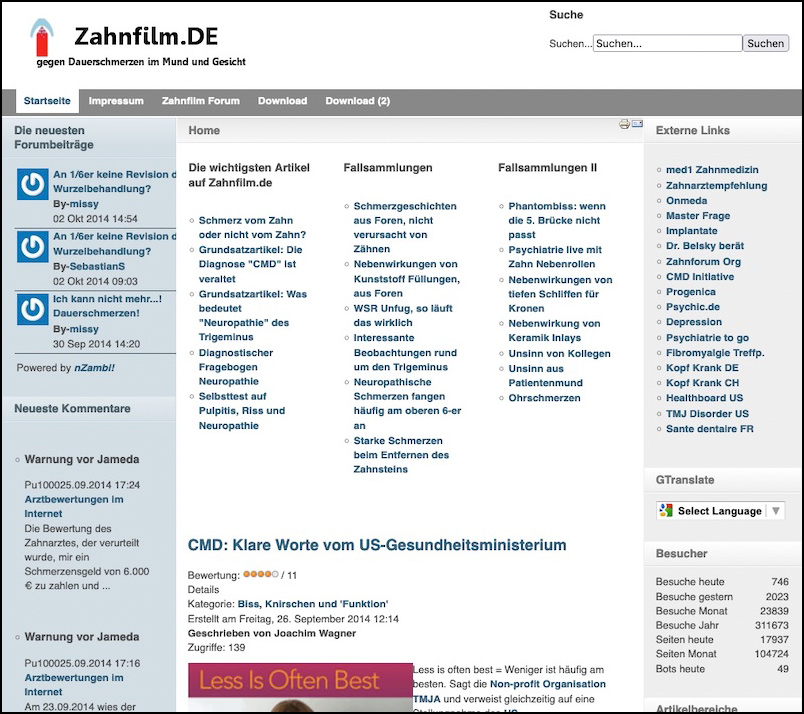
Hier findet man allerlei Informationen, die zum Thema gehören, aber auch zur Zahnmedizin allgemein und auch viele praktische Quellen. Das Forum eignet sich als Ort zum Austausch, in dem auch Laien ihre Fragen zu Gehör bringen können. Alles zur Seite und den interessanten Inhalten gibt es in diesem Artikel zu erfahren.
Zahnfilm – die Webseite über Zahnmedizin
Zahnfilm.de – die Webseite mit ausführlichen Informationen über Zahnmedizin
Zahnschmerzen mag wohl niemand gerne. Selbst wenn sie gar nicht so stark ausfallen, können sie sich doch als sehr nervig entpuppen, vor allem auch dann, wenn es chronisch wird. Bei chronischen Schmerzen muss man ohnehin genauer hinschauen. In keinem Fall sollte man solche Schmerzen ignorieren, ob nun direkt an den Zähnen oder auch im Kiefer. Der erste Schritt kann dabei durchaus sein, dass man sich selbst Informationen einholt, wofür das Internet ideal ist. Jedoch kann man auch viele falsche Informationen finden oder auch richtige, die aber gar nicht auf den eigenen Fall zutreffen. Insofern bietet sich in Sachen Zahnfragen die Webseite zahnfilm.de an, denn hier gibt es nicht nur die Informationen an sich, sondern auch ein Forum, in dem man Fragen stellen kann.
Die Webseite Zahnfilm wird vom Zahnarzt Joachim Wagner betrieben, der so eine großartige Quelle zu Zahnfragen aufgebaut hat. Schon die Startseite zeigt, dass es hier in erster Linie um Informationen geht. In einer Datenbank kann man jede Menge Informationen zu unterschiedlichen Anliegen finden, wobei gerade auch der Kiefer im Fokus steht. Darüber hinaus gibt es aber auch noch das Forum, das den Austausch zwischen Fachleuten und auch Laien ermöglicht. Um darin schreiben zu können, muss man sich kostenlos registrieren und kann danach beliebig schreiben und seine Fragen loswerden. Egal ob zu Wurzelbehandlungen, Milchzähnen oder etwas thematischem Verwandtes.
Auf der linken Seite findet sich das Menü der Inhalte, sodass man direkt darauf klicken kann, um nähere Informationen zu erhalten. Beispielsweise allgemeine Texte zu chronischen Zahnschmerzen, zu Füllungsmaterial, Wurzelbehandlungen, Karies oder auch generell Patienten oder Depressionen. Die Vielfalt der Artikel ist groß. Darüber hinaus gibt es außerdem auch eine lange Liste von guten Quellen zu anderen Seiten, die sich in irgendeiner Weise mit der Zahnmedizin und verwandten Themen beschäftigen. Diese lassen sich auf der rechten Seite finden.
Fokus auf chronische Kieferschmerzen
Schmerzen im unteren Kopfbereich müssen nicht zwangsläufig Zahnschmerzen sein. Häufig gibt es auch Kieferschmerzen, die sich zu einem chronischen Problem entwickeln und so auch einen großen Leidensdruck verursachen. Natürlich kann man zum Zahnarzt gehen, wenn man sich nicht sicher ist, oder aber direkt zum Kieferorthopäden, der die richtige Adresse für solche Probleme darstellt. Von chronischen Schmerzen im Kiefergelenk spricht man schon dann, wenn sie über eine Woche lang anhalten. Insofern sollte man nicht allzu lange warten, wenn man Symptome hat, selbst wenn sich diese als harmlos herausstellen sollten. Unbehandelte Kieferprobleme können zu Folgeschäden führen, die umso schwerer zu behandeln sind und sich auch über den Kieferbereich hinaus ausdehnen können.
Kieferschmerzen können bei verschiedenen Handlungen auftreten, beispielsweise Sprechen, Kauen oder auch Abbeißen. Insofern bleiben sie auch meist nicht lange unentdeckt. Diese Schmerzen entstehen meist aufgrund des Umstands, dass sich der bewegliche Unterkiefer im Gegensatz zum unbeweglichen Oberkiefer bewegt. Verbunden sind diese beiden Elemente über eine Gelenkgrube. Wenn hier ein Defekt am Knorpel vorliegt, kann es zu Problemen kommen. Oft treten Schmerzen und Probleme durch eine Überbelastung auf.
Symptome, die durch Kieferprobleme auftreten können, sind unter anderem Schmerzen, die eben im Kiefer oder auch im Gesicht, dem Kopf und Nacken auftreten. Es kann auch Reibungs- und Knackgeräusche geben, die zwar nicht wehtun, aber auf Probleme hinweisen. Schwellungen, Blockierungen und Verspannungen sind ebenfalls oft zu bemerken. Diese können sich auf viele Bereiche des Körpers ausdehnen, sowohl dem Nacken, den Schultern, als auch dem Rücken, der Hüfte und sogar den Knien. Taubheitsgefühle in den Fingern können ebenfalls ihre Ursache im Kiefer haben.
Neuropathische Zahnschmerzen
Neuropathischer Zahnschmerz unterscheidet sich von anderen Zahnschmerzen. Er entsteht, wenn Nerven im Mund beschädigt sind. Diese Beschädigungen können durch Eingriffe, Infektionen oder Verletzungen verursacht werden. Im Gegensatz zu anderen Zahnschmerzen hat er oft keinen klaren Auslöser. Oft erscheint der Schmerz spontan. Er kann brennend, stechend oder kribbelnd sein. Solche Empfindungen sind für neuropathische Schmerzen typisch. Sie können plötzlich auftreten und ebenso plötzlich verschwinden. Da sie schwer zu lokalisieren sind, ist die Diagnose oft kompliziert. Deshalb ist ein gründlicher Zahnarztbesuch wichtig. Er kann feststellen, ob der Schmerz wirklich neuropathisch ist. Eine genaue Diagnose hilft bei der Auswahl der richtigen Behandlung. Medikamente oder spezielle Therapien können helfen. Das Ziel ist, den Schmerz zu lindern und die Lebensqualität zu verbessern.
Fazit zur Zahnfilm Webseite
Zahnschmerzen und insbesondere Kieferschmerzen können das tägliche Leben erheblich beeinträchtigen. Daher ist es wichtig, gut informiert zu sein und Probleme rechtzeitig zu erkennen. Wer sich generell zum Thema, Symptomen und Problemen informieren möchte, findet gute Informationen auf der Seite Zahnfilm.de, die kostenlos genutzt werden kann. Hier werden nicht nur Details zu allgemeinen Zahnthemen behandelt, sondern auch spezielle Problembereiche wie chronische Kieferschmerzen und neuropathische Zahnschmerzen. Darüber hinaus bietet das Forum eine Plattform für den Austausch und die Klärung individueller Anliegen. Ebenso wichtig ist es, Symptome nicht zu ignorieren und bei anhaltenden Schmerzen professionelle Hilfe zu suchen. Schließlich kann die richtige Diagnose und Behandlung den Unterschied zwischen Leiden und einem schmerzfreien Leben ausmachen.